Introduction:
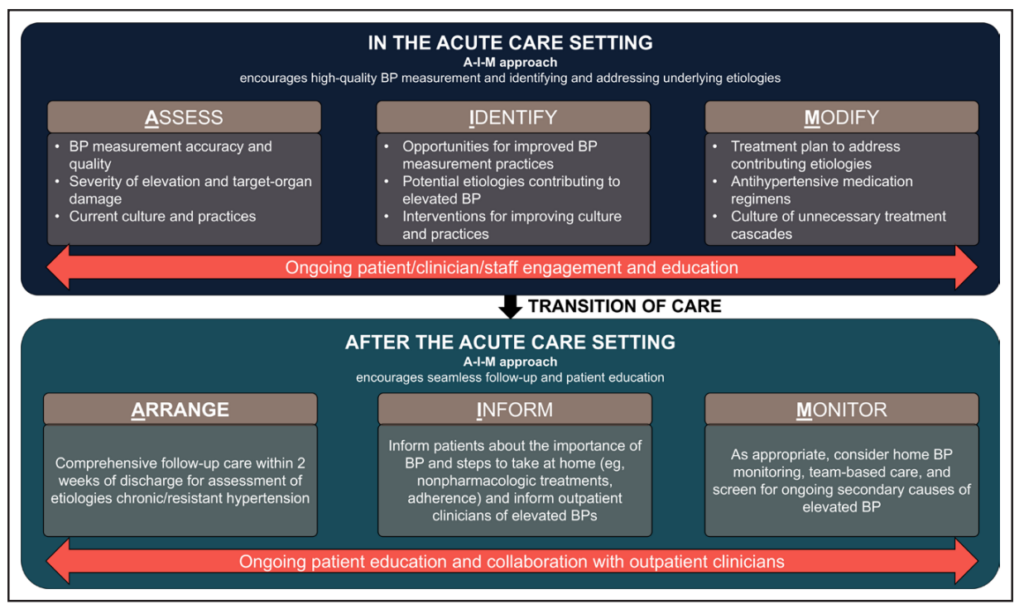
The management of elevated inpatient blood pressure (BP) requires a structured approach to ensure patient safety and effective care. It involves accurate BP measurement, assessing the severity of the elevation, evaluating for target-organ damage, addressing underlying causes, and carefully balancing the risks and benefits of initiating antihypertensive treatment. Using structured acronyms such as A-I-M (Assess, Identify, Modify) for inpatient management and A-I-M (Arrange, Inform, Monitor) for post-discharge care provides a practical framework.
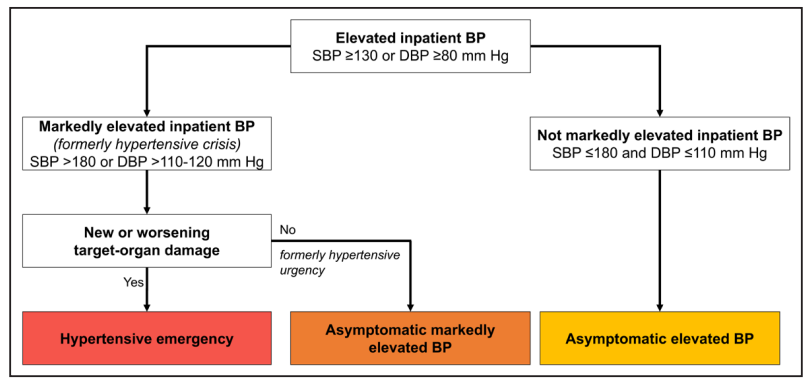
Proper differentiation between hypertensive emergencies and asymptomatic elevated BP is critical, as each scenario demands distinct evaluation and treatment strategies.
General Approach
Management involves:
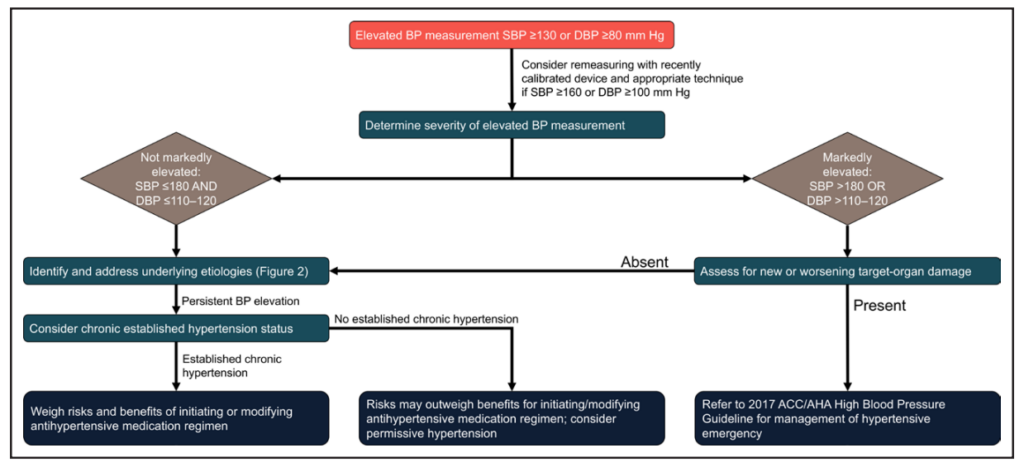
- Accurate BP measurement and reassessment.
- Evaluating for target-organ damage.
- Identifying and addressing underlying causes.
- Careful decision-making regarding antihypertensive treatment, considering risks and benefits
The A-I-M framework is suggested:
- In-hospital: Assess, Identify, Modify.
- Post-discharge: Arrange, Inform, Monitor.
Hypertensive Emergency
- Defined by markedly elevated BP with evidence of new or worsening target-organ damage.
- Key areas to evaluate: Brain, Arteries, Retina, Kidneys, Heart (BARKH).
- Steps include:
- Detailed history (e.g., chronic hypertension, adherence to medications).
- Comprehensive physical examination.
- Investigations like metabolic panels, ECG, chest X-ray, and volume assessment.
- Treatment follows the 2017 Hypertension Clinical Practice Guidelines, often involving prompt initiation of antihypertensives.
Asymptomatic Elevated Inpatient BP
- More common than hypertensive emergency, with unclear treatment guidelines.
- PRN orders for intravenous antihypertensives are discouraged due to risks, including:
- BP fluctuations.
- Morning hypotension delaying oral medications.
- Increased BP variability.
Key Recommendations:
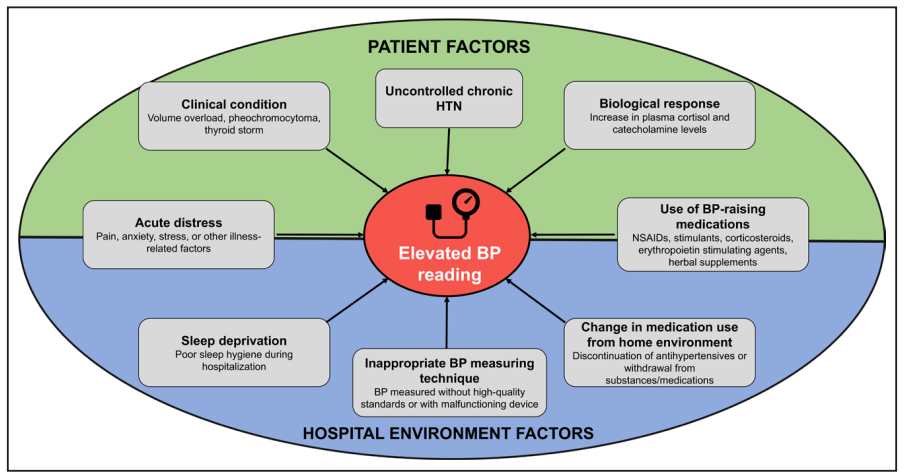
- Verify measurement accuracy: Ensure proper technique and device calibration.
- Identify reversible causes: Pain, stress, medications (e.g., NSAIDs, corticosteroids), and fluid imbalance.
- Consider home BP management: Review adherence and appropriateness of home antihypertensive regimens.
- Avoid PRN intravenous medications for asymptomatic elevated BP unless strongly indicated.
Risks of Over-Treating Asymptomatic Elevated BP
- No RCT evidence supports treatment benefits in asymptomatic patients.
- Observational studies show:
- Increased risks with intravenous medications, including acute kidney injury, myocardial injury, and hypotension.
- PRN treatments often result in abrupt BP drops, leading to adverse outcomes:
- 60% higher risk of myocardial injury.
- 2-fold higher mortality risk.
- Risk of abrupt BP reductions (>25% drop).
Conclusion
In managing asymptomatic elevated BP, focus on:
- Proper measurement and identifying reversible factors.
- Avoiding unnecessary PRN antihypertensives.
- Individualized care that minimizes risks, especially in acute hospital settings.

Leave a Reply
You must be logged in to post a comment.