Introduction:
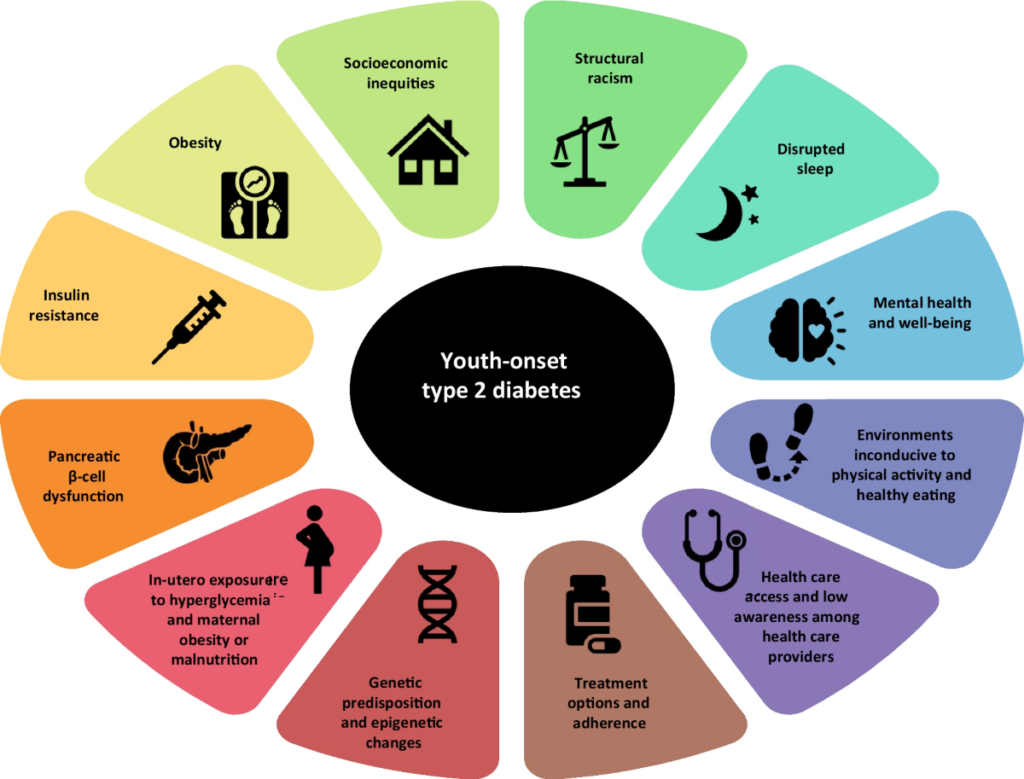
Type 2 diabetes (T2DM) in children and adolescents has become a significant concern, particularly given its link to obesity and potential long-term vascular complications, similar to adult-onset diabetes. Pediatric T2DM differs from adult-onset disease in that it often has more aggressive progression, including difficulties in maintaining long-term glycemic control and earlier complications.
The TODAY study, a large clinical trial, found that oral monotherapy with agents like metformin does not provide durable control, highlighting the need for a combination of pharmacologic and non-pharmacologic interventions. Multidisciplinary care involving endocrinologists, dietitians, mental health professionals, and others is recommended, though primary care providers may manage patients where resources are limited.

Goals of Management
Improve Glycemic Control: This involves monitoring blood glucose levels through fasting or random plasma glucose tests, oral glucose tolerance tests, or hemoglobin A1c (HbA1c).
Address Obesity: Since most youth with T2DM are obese or overweight, managing weight is key. Obesity is linked to insulin resistance, which worsens glycemic control.
Address Comorbidities: Comorbid conditions like hypertension, dyslipidemia, and liver disease (e.g., metabolic dysfunction-associated steatotic liver disease) should be identified and treated.
Prevent Long-term Vascular Complications: The long-term goal is to prevent complications associated with T2DM, particularly vascular damage.
Nonpharmacologic Therapy:
Weight Reduction: A cornerstone of managing T2DM in youth, as excess weight worsens insulin resistance. Weight reduction improves both insulin sensitivity and glycemic control.
Weight goals:
For those who have completed growth, a 7-10% reduction in body weight is ideal. For growing children, the goal is to reduce BMI to less than the 85th percentile for age and sex
- Moderate Weight Loss: A gradual approach is recommended, aiming for 0.5 to 1 kg weight loss per month for growing adolescents, or 0.5 to 1 kg per week for those who have completed puberty.
- Dietary Changes: A balanced, reduced-calorie diet is essential, with consultation from a dietitian to develop personalized nutrition plans. This includes decreasing portion sizes, eliminating high-calorie beverages, and reducing fast food consumption.
- Physical Activity: Regular exercise, regardless of weight loss, improves insulin sensitivity.
Recommendation: Youth should aim for at least 1 hour of moderate-to-vigorous physical activity daily, including strength training at least three times a week, and limiting sedentary activities (e.g., screen time) to less than 2 hours per day.
- Dietary Counseling: Counseling should focus on sustainable, family-based dietary changes rather than rigid meal planning. Involvement of the child and family is crucial for adherence.
Guidance:
Decrease portion sizes and replace high-calorie foods with healthier options (e.g., fruits, vegetables). Eliminate sugary drinks and replace them with water or calorie-free beverages. Increase home-cooked family meals and reduce eating out.
Behavioral Support: Frequent visits to dietitians or healthcare providers (every 4 weeks) are necessary to reinforce healthy behaviors. Additionally, mental health professionals may help address the psychological challenges of managing diabetes in youth.
Other Guidance:
Screening for Risk Behaviors: Regular counseling should be provided for high-risk behaviors such as smoking, vaping, and alcohol use, as these can exacerbate T2DM complications.
Pharmacologic Agents for Managing Type 2 Diabetes Mellitus (T2DM) in Children and Adolescents
Pharmacologic Therapy:
While metformin is the first-line pharmacologic treatment for T2DM in youth, it may need to be supplemented with other medications or therapies if glycemic control is not achieved. Referral to a specialist or endocrinologist should be made if control is not reached with metformin alone.
1. Primary Therapy Options:
- Metformin: First-line therapy for most pediatric patients with T2DM, used alongside nonpharmacologic treatments like diet and exercise.
Mechanism: Improves insulin sensitivity by increasing insulin-mediated glucose uptake in peripheral tissues and decreasing hepatic glucose production.

Additional Benefit: Promotes modest weight loss, which contrasts with weight gain associated with insulin, thiazolidinediones, or sulfonylureas.
- Insulin:
Used when: Patients present with ketosis, severe hyperglycemia, or mixed features of type 1 and type 2 diabetes.
Indicated when: Random plasma glucose is ≥250 mg/dL or HbA1c is >9%. A significant proportion of youth with T2DM will eventually need insulin therapy.
Role: Insulin is essential when beta cell function is insufficient due to insulin resistance.

2. Second-Line Therapy Options:
- GLP-1 Agonists (Liraglutide, Extended-Release Exenatide, Dulaglutide): FDA-Approved for pediatric use (≥10 years old) to support glycemic control alongside diet and exercise.
Mechanism: Incretin mimetics that boost glucose-dependent insulin secretion and improve insulin response after meals.
Benefits: May promote modest weight loss through delayed gastric emptying and appetite regulation. Potential cardiovascular benefits (from adult studies). .
- Semaglutide: Another long-acting GLP-1 agonist, FDA-approved for adults and adolescents with T2DM or for weight management.
- Sodium-Glucose Cotransporter 2 (SGLT2) Inhibitors (e.g., canagliflozin, dapagliflozin): Investigated in pediatric T2DM, with some positive outcomes leading to FDA approval for certain agents in specific age groups.
Mechanism: Increase urinary glucose excretion, thereby reducing blood glucose levels and promoting weight loss. Side Effects: Increased risk of diabetic ketoacidosis (DKA). SGLT2 inhibitors have shown positive results for cardiorenal outcomes in adults.
In conclusion, managing type 2 diabetes in children and adolescents requires a comprehensive, multidisciplinary approach that combines pharmacologic treatment with lifestyle modifications. Weight reduction, dietary changes, and regular physical activity are essential nonpharmacologic strategies, while pharmacologic agents like metformin, insulin, and GLP-1 agonists may be necessary for achieving glycemic control. The aggressive nature of pediatric T2DM necessitates early intervention, ongoing monitoring, and support from healthcare professionals, including dietitians and mental health experts, to address both the physical and psychological aspects of the disease. Effective management not only aims to control blood glucose but also to prevent long-term complications such as vascular damage and to improve overall quality of life for affected youth.
Source-

Leave a Reply
You must be logged in to post a comment.